If you have celiac disease, understanding gluten isn’t optional—it’s survival. Gluten is everywhere, often hiding in foods you’d never suspect. This guide goes beyond the basics to explain what gluten actually is, exactly how it damages your body, and why the FDA’s “gluten-free” standard may not be strict enough for everyone with celiac disease.
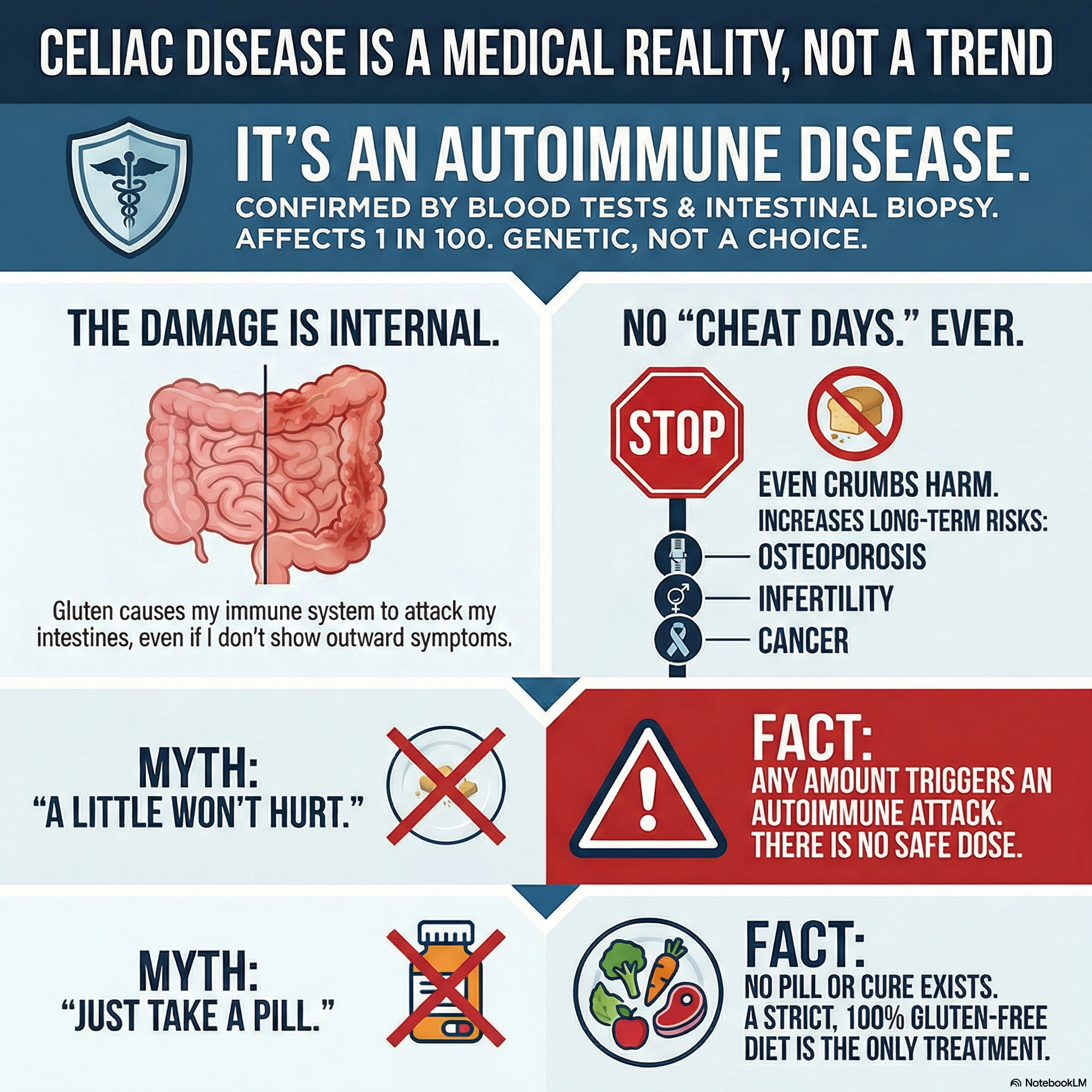 Understanding why celiac disease is an autoimmune condition—not a food preference
Understanding why celiac disease is an autoimmune condition—not a food preference
What Is Gluten, Exactly?
 Gluten forms an elastic protein network that gives bread its structure
Gluten forms an elastic protein network that gives bread its structure
Gluten isn’t a single substance—it’s a family of storage proteins found in certain grains. The name comes from the Latin word for “glue,” describing its sticky, elastic properties when mixed with water.
The Two Proteins That Matter
Gluten consists of two main protein groups:
Gliadin (α, β, γ, ω variants)
- The primary trigger for the celiac immune response
- Alcohol-soluble (which is why some extraction tests use alcohol)
- Contains the specific peptide sequences that activate celiac T-cells
- Research shows the 33-mer gliadin peptide is particularly immunogenic
Glutenin (high and low molecular weight)
- Provides elasticity and strength to dough
- Less immunogenic than gliadin but still problematic
- Responsible for bread’s chewy texture
When flour meets water, these proteins bond together, forming the stretchy network that traps carbon dioxide during baking and gives bread its structure.
Why Your Immune System Attacks It
In celiac disease, your immune system recognizes specific amino acid sequences in gliadin as threats. The mechanism works like this:
- Gliadin peptides cross the intestinal barrier
- The enzyme tissue transglutaminase (tTG) modifies the gliadin
- This modification makes gliadin fit perfectly into HLA-DQ2/DQ8 molecules on immune cells
- T-cells recognize this complex and initiate an inflammatory attack
- The attack targets not just the gluten but your own intestinal tissue
This is why celiac disease is autoimmune—your body attacks itself in response to gluten.
Where Is Gluten Found?
Primary Sources (Always Contain Gluten)
Wheat (Triticum species) — The dominant source in Western diets
- Bread wheat (Triticum aestivum)
- Durum wheat (pasta, couscous)
- Spelt (T. spelta)
- Kamut/Khorasan
- Einkorn (T. monococcum)
- Emmer/Farro (T. dicoccum)
- Bulgur, semolina, wheat berries
Barley (Hordeum vulgare) — Contains hordeins
- Beer and lagers (unless specifically GF)
- Malt, malt extract, malt flavoring
- Malt vinegar
- Barley flour
- Many breakfast cereals
Rye (Secale cereale) — Contains secalins
- Rye bread, pumpernickel
- Rye crackers
- Some whiskeys (though distillation may remove gluten proteins)
Triticale — Wheat-rye hybrid, contains both types
Hidden Sources: Where Gluten Lurks
This is where most people with celiac disease get “glutened.” According to Beyond Celiac, hidden gluten is the leading cause of ongoing symptoms.
In the Kitchen:
- Soy sauce (most brands contain wheat—use tamari or coconut aminos)
- Worcestershire sauce (traditional recipes contain malt vinegar)
- Salad dressings (flour thickeners, malt vinegar)
- Gravies and cream sauces (flour thickeners)
- Soups (flour thickeners, barley)
- Marinades (soy sauce, beer)
Processed Foods:
- Processed meats (wheat fillers, binders, flavorings)
- Imitation seafood (surimi often contains wheat)
- Flavored chips and snacks (wheat-based seasonings)
- Candy (malt, wheat starch, cookie pieces)
- Ice cream (cookie/brownie flavors, thickeners)
- Protein bars (often contain wheat/barley)
Non-Food Sources (Cross-Contact Risk):
- Medications and supplements (use GlutenFreeDrugs.com to verify)
- Lipstick and lip balm
- Communion wafers
- Play-Doh (children’s hand-to-mouth contact)
- Pet food (handling dry kibble)
- Envelope adhesive (traditional)
- Stamps (traditional)
Naturally Celiac-Safe Grains
These grains do NOT contain gluten proteins:
| Grain | Notes |
|---|---|
| Rice (all varieties) | Naturally safe |
| Corn/maize | Naturally safe |
| Quinoa | Naturally safe; some brands test for cross-contact |
| Buckwheat | Despite the name, NOT wheat |
| Millet | Naturally safe |
| Amaranth | Naturally safe |
| Teff | Naturally safe |
| Sorghum | Naturally safe |
| Oats | Only if certified GF — conventional oats are heavily cross-contaminated |
Warning about oats: Even “pure” oats may trigger reactions in some people with celiac disease due to avenin, a similar protein. Introduce cautiously and monitor for symptoms.
How Gluten Damages the Celiac Intestine
Understanding the damage mechanism helps you understand why even trace amounts matter.
The Damage Cascade
 From healthy villi to complete flattening—each gluten exposure causes measurable damage
From healthy villi to complete flattening—each gluten exposure causes measurable damage
- Gluten Ingestion — Even 50mg of gluten (about 1/100th of a slice of bread) can trigger a response
- Intestinal Permeability — Gluten increases zonulin production, opening tight junctions between cells
- tTG Modification — Tissue transglutaminase modifies gliadin peptides
- Immune Recognition — HLA-DQ2/DQ8 molecules present modified gliadin to T-cells
- Inflammatory Response — T-cells release cytokines; B-cells produce antibodies
- Villous Destruction — Inflammation destroys villi, reducing nutrient absorption
- Crypt Hyperplasia — Intestinal crypts elongate trying to compensate
- Ongoing Damage — Process repeats with each gluten exposure
The 20 PPM Question: Is FDA “Gluten-Free” Safe Enough?
The FDA’s gluten-free standard allows up to 20 parts per million (ppm) gluten. But is this safe for everyone with celiac disease?
The research says… it depends:
| Study | Finding |
|---|---|
| Catassi et al., 2007 | 10mg/day gluten caused mucosal damage in some patients |
| Akobeng & Thomas, 2008 | Threshold varies; some react to <10 ppm |
| FDA Rationale | 20 ppm is “reliably detectable” and “safe for most” |
What this means for you:
- 20 ppm is a minimum standard, not optimal
- If you’re symptomatic despite a “gluten-free diet,” accumulated low-level exposure may be the cause
- GFCO certification (<10 ppm) provides an extra safety margin
- Dedicated facility products offer the highest safety
Celiac-Safe Standards Compared
| Certification | Gluten Threshold | Testing Required |
|---|---|---|
| FDA “Gluten-Free” | <20 ppm | Manufacturer’s responsibility |
| GFCO | <10 ppm | Third-party testing |
| NSF Gluten-Free | <20 ppm | Third-party testing |
| Celiac Support Association (CSA) | <5 ppm | Third-party testing |
| Dedicated Facility | Ideally 0 | Varies |
Cross-Contact: The Invisible Threat
Cross-contact (sometimes called cross-contact) occurs when celiac-safe food touches gluten-containing food, surfaces, or utensils. For people with celiac disease, this is often the difference between safety and weeks of symptoms.
Common Cross-Contact Points
In Home Kitchens:
- Shared toasters (crumb trays hold gluten indefinitely)
- Wooden cutting boards and spoons (absorb gluten)
- Shared butter/peanut butter jars (knife double-dipping)
- Colanders (gluten pasta residue)
- Cast iron pans (if seasoned with flour)
- Shared cooking oil (flour particles)
In Restaurants:
- Shared fryers (breaded items + fries = contaminated fries)
- Grill surfaces (burger buns + naked patties)
- Pasta water (shared boiling water)
- Pizza ovens (shared surfaces)
- Garnishes (croutons removed ≠ safe salad)
- Server/chef glove changes
In Manufacturing:
- Shared equipment lines
- Airborne flour particles
- Shared storage facilities
- Same-day production sequencing
Cross-Contact Prevention Protocol
At Home:
- Designate dedicated celiac-safe utensils (color-coded)
- Store gluten-free products above gluten products (prevents falling crumbs)
- Use squeeze bottles for shared condiments
- Have a dedicated toaster or use toaster bags
- Clean surfaces with soap and water (not just wiping)
- Consider a dedicated celiac-safe section of the kitchen
Dining Out:
- Research restaurants in advance (Find Me Gluten Free app)
- Call ahead during non-rush hours
- Ask specific questions: “Do you have a dedicated fryer?” “Is there a separate prep area?”
- Communicate that it’s a medical condition, not a preference
- Tip well and build relationships with safe restaurants
Testing for Gluten
Food Testing Methods
ELISA (Enzyme-Linked Immunosorbent Assay)
- Industry standard for gluten detection
- Can detect down to 3-5 ppm
- R5 antibody specifically targets toxic peptides
- R5 ELISA is internationally validated
Consumer Testing Devices
- Nima Sensor: Tests individual portions; useful but has limitations (false negatives possible in fermented products)
- EZ Gluten: Home test strips
- GlutenTox: Professional and home testing kits
Limitations of Testing:
- Tests sample only a small portion of food
- Fermented products may show false negatives
- “Not detected” ≠ “zero gluten”
- Testing should complement, not replace, careful selection
Medical Testing for Exposure
If you suspect you’ve been glutened, these tests can help:
- tTG-IgA: Rises after exposure, peaks 2-4 weeks later
- DGP-IgA/IgG: May rise earlier than tTG
- Intestinal biopsy: Gold standard but invasive; not practical for routine monitoring
Myths vs. Facts
Myth: “A little gluten won’t hurt if I don’t feel symptoms”
Fact: Studies show intestinal damage occurs even without symptoms. “Silent” damage increases long-term complications including osteoporosis, infertility, and lymphoma.
Myth: “Gluten-free is healthier for everyone”
Fact: For people without celiac disease or NCGS, there’s no evidence of benefit. gluten-free products are often lower in fiber, higher in sugar, and less fortified.
Myth: “Wheat-free means gluten-free”
Fact: Wheat-free products may contain barley, rye, or cross-contaminated oats. Always verify “gluten-free,” not just “wheat-free.”
Myth: “Cooking destroys gluten”
Fact: Gluten proteins are heat-stable. Baking, frying, and boiling do NOT eliminate gluten. Only enzymatic degradation (not practical in cooking) breaks down the problematic peptides.
Myth: “I can tell when I’ve been glutened”
Fact: Many people have “silent” celiac disease with no noticeable symptoms despite ongoing damage. Symptoms are not a reliable indicator of exposure—up to 50% of gluten exposures may be asymptomatic.
Building a Celiac-Safe Life
Step 1: Audit Your Kitchen
Identify and address all cross-contact risks. Consider a full kitchen “reset” after diagnosis.
Step 2: Learn to Read Labels
- Look for “gluten-free” labeling AND certification logos
- Check “Contains” and “May contain” statements
- Research unfamiliar ingredients
- Re-check products periodically (formulations change)
Step 3: Build Your Safe Food List
- Identify trusted brands with third-party certification
- Find local restaurants with genuine celiac-safe protocols
- Stock naturally gluten-free whole foods as your foundation
Step 4: Prepare for Social Situations
- Eat before events where safe food isn’t guaranteed
- Bring your own food when appropriate
- Practice explaining your needs clearly and confidently
Step 5: Monitor Your Health
- Regular follow-up with celiac-knowledgeable healthcare provider
- Annual tTG-IgA to monitor dietary compliance
- Nutritional testing for common deficiencies
Conclusion
Understanding gluten at a deeper level—what it is chemically, how it triggers your immune system, where it hides, and how cross-contact occurs—is fundamental to celiac-safe living.
The difference between “gluten-free” and “celiac-safe” often comes down to this knowledge. A lifestyle dieter can get away with 20 ppm products and shared fryers. You can’t.
Your health depends on understanding that every exposure matters, that hidden gluten is everywhere, and that “gluten-free” on a label is a starting point—not a guarantee.
This content is for educational purposes only. Always consult with a healthcare provider for medical advice specific to your condition.
Sources
- Green PHR, Cellier C. “Celiac Disease.” New England Journal of Medicine. 2007;357(17):1731-1743.
- Catassi C, et al. “A prospective, double-blind, placebo-controlled trial to establish a safe gluten threshold for patients with celiac disease.” American Journal of Clinical Nutrition. 2007;85(1):160-166.
- Akobeng AK, Thomas AG. “Systematic review: tolerable amount of gluten for people with coeliac disease.” Alimentary Pharmacology & Therapeutics. 2008;27(11):1044-1052.
- FDA. “Questions and Answers: Gluten-Free Food Labeling Final Rule.” August 2013.
- Thompson T, et al. “gluten cross-contact of grains, seeds, and flours in the United States.” Journal of the American Dietetic Association. 2010.
- Silano M, et al. “Diversity of oat varieties in eliciting the early inflammatory events in celiac disease.” European Journal of Nutrition. 2014.
- Beyond Celiac. “Sources of Gluten.” Accessed January 2026.