 Your quick guide to being there for them
Your quick guide to being there for them
First: This Isn’t Your Fault
If your child was just diagnosed with celiac disease, you might be wondering what you did wrong. You did nothing wrong. Celiac disease is genetic—it was always going to happen if the right combination of genes and environmental triggers came together.
If your partner, parent, sibling, or friend was diagnosed, you might feel helpless or unsure how to help. The fact that you’re reading this means you’re already doing the right thing.
This guide will give you everything you need to support your loved one safely and effectively.
Part 1: Understanding What They’re Going Through
What Celiac Disease Actually Is
Celiac disease is an autoimmune condition, not an allergy or intolerance. When someone with celiac eats gluten (a protein in wheat, barley, and rye), their immune system attacks their own small intestine.
Key points to understand:
- It’s lifelong—there’s no cure, no growing out of it
- The only treatment is a strict gluten-free diet
- Even tiny amounts of gluten cause damage (we’re talking breadcrumb-level)
- Damage occurs whether or not they have symptoms
- It’s genetic—if one family member has it, others might too
What Your Loved One Is Feeling
Beyond the physical symptoms, a celiac diagnosis brings emotional weight:
For children:
- Fear of being “different” from their friends
- Anxiety about birthday parties, school lunch, sleepovers
- Sadness about missing their favorite foods
- Worry about being a burden
- Confusion about why their body “doesn’t work right”
For adults:
- Grief over lost foods and spontaneity
- Frustration with the learning curve
- Anxiety about social situations and dining out
- Concern about being a burden to loved ones
- Overwhelm from the constant vigilance required
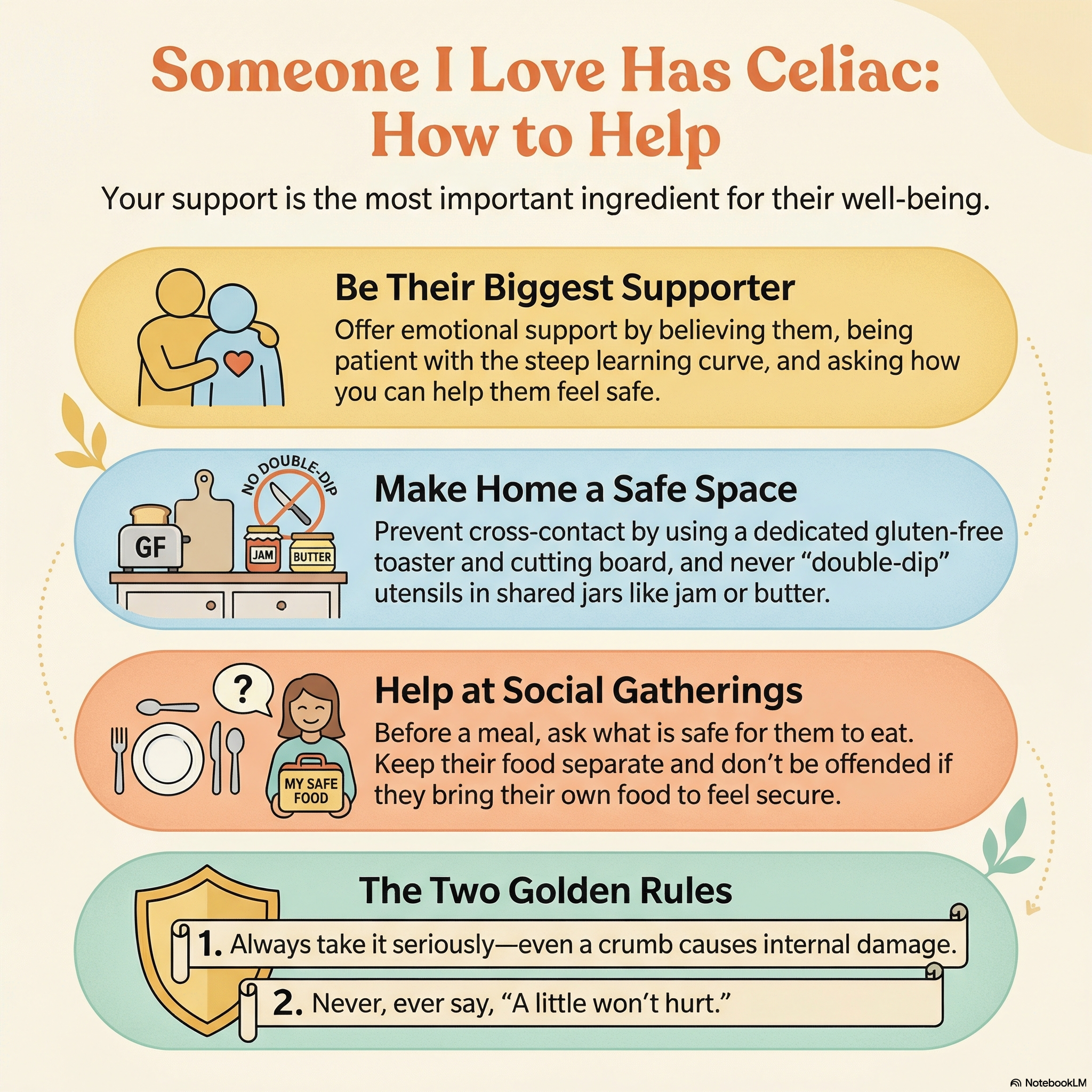
What They Need From You
- Belief — Take their condition seriously, always
- Patience — Learning to live gluten-free takes time
- Support — Help with meal prep, label reading, and advocacy
- Flexibility — Adjust family routines to keep them safe
- Normalcy — Don’t make them feel like a burden or “other”
Part 2: Keeping Them Safe at Home
 Setting up a safe kitchen is essential for protecting your loved one
Setting up a safe kitchen is essential for protecting your loved one
Kitchen Setup: The Basics
Option A: Fully Gluten-Free Kitchen This is the safest option, especially with young children:
- Remove all gluten-containing products
- Everyone eats gluten-free at home
- Gluten only enters when eating out
Option B: Shared Kitchen with Designated Areas If going fully gluten-free isn’t possible:
- Designate separate shelves/cabinets for gluten-free items
- Use color-coded equipment (e.g., red cutting board = gluten-free only)
- Store gluten-free items ABOVE gluten items (crumbs fall down)
- Establish clear rules about cross-contact
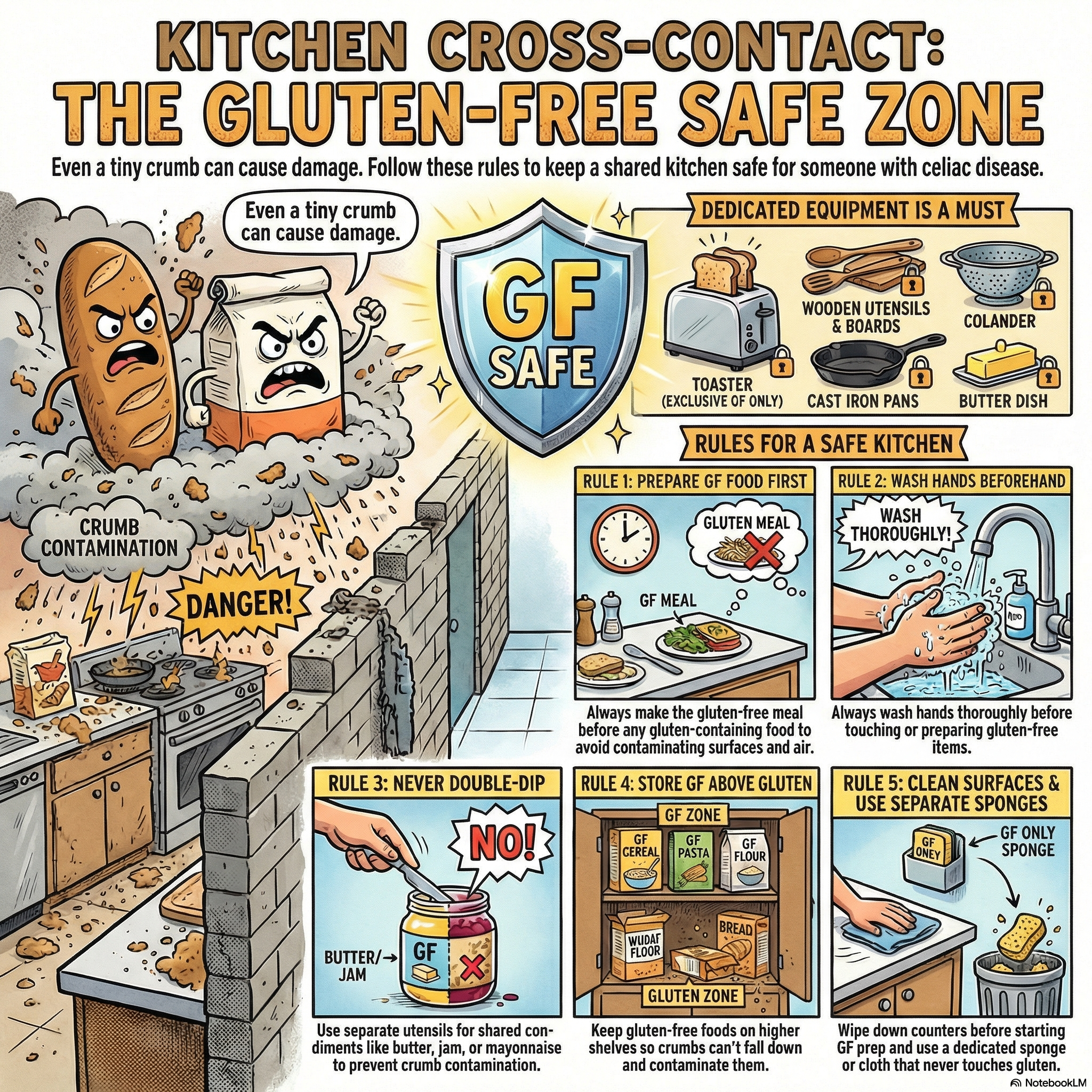
Must-Have Dedicated Equipment
These items CANNOT be safely shared:
- Toaster (crumbs are impossible to remove)
- Cutting boards (especially wood—they harbor gluten)
- Colander/strainer (mesh traps particles)
- Wooden utensils (porous, absorb gluten)
- Butter dish (crumbs from knives)
- Condiment containers (if double-dipping occurs)
- Cast iron (seasoning can trap gluten)
Cross-Contact Prevention Rules
Teach everyone in the household:
- Always prepare gluten-free food FIRST (before flour is in the air)
- Wash hands before touching gluten-free items
- Never double-dip — use clean utensils for each container
- Keep gluten-free food covered when gluten is being prepared
- Clean surfaces thoroughly before preparing gluten-free food
- Use separate sponges (or wash gluten dishes last)
The “Flour Tornado” Problem
When you open a bag of flour or bake with wheat flour, gluten particles become airborne and settle on every surface within a large radius. They can remain for hours.
Solutions:
- Do gluten baking when your celiac family member isn’t home
- Clean all surfaces, counters, and nearby items thoroughly after
- Or better yet: switch to gluten-free baking for everyone
Part 3: For Parents of Celiac Children
Making Them Feel Normal, Not Broken
Children with celiac can easily feel “broken” or “different.” Your language matters:
SAY: “Your body works differently—it’s really good at telling you what’s not good for it.”
DON’T SAY: “You can’t eat that because you’re sick.”
SAY: “Let’s find a delicious gluten-free version of that!”
DON’T SAY: “Sorry, that has gluten. You can’t have it.”
SAY: “You have a superpower—you know exactly how to keep yourself healthy.”
DON’T SAY: “It must be so hard for you to watch everyone else eat pizza.”
School and Daycare
Before school starts, provide:
- Written documentation of diagnosis (doctor’s note)
- A 504 Plan or similar accommodation plan (in the US)
- List of safe snacks for emergencies
- Emergency contact procedures if they’re exposed
- Safe treats they can have during class parties
The 504 Plan should include:
- Safe food storage area
- Permission to carry safe snacks
- Accommodations for field trips
- Procedures for art projects (Play-Doh, pasta art, etc.)
- Staff training requirements
- Emergency protocols
Questions to ask the school:
- How will lunch be handled? (Separate prep area?)
- Who will supervise to ensure no food sharing?
- What’s the policy on classroom snacks and parties?
- How will art projects with wheat-based materials be handled?
- What happens on field trips?
Birthday Parties and Playdates
For parties your child attends:
- Contact the host in advance
- Offer to send safe alternatives (same thing but GF)
- Send a safe cupcake they can have when cake is served
- Educate the host on cross-contact basics
- Stay at the party if possible, or ensure a knowledgeable adult is there
For parties you host:
- Consider making the whole party gluten-free (often no one notices)
- If serving gluten items, serve them last and separately
- Have a clear “safe zone” for your child’s food
- Label foods clearly
For sleepovers:
- Send all food they’ll need (breakfast, snacks, treats)
- Create a “food instruction card” for the host parents
- Consider hosting sleepovers at your house instead
Talking to Other Parents
Give them a brief explanation and clear instructions:
“[Child’s name] has celiac disease—an autoimmune condition where gluten (in wheat, barley, and rye) damages their intestines. It’s not an allergy, and even tiny amounts cause harm. I’ll send all the food they need. The most important thing is making sure they only eat what I send and that it doesn’t touch other food. Thank you for helping keep them safe!”
Managing Their Emotional Well-being
Watch for signs of:
- Food anxiety (fear of eating anything)
- Depression or withdrawal
- Anger about their condition
- Obsessive behavior around food
- Eating secretly or avoiding food
If you see these signs:
- Talk openly about their feelings
- Connect them with other celiac kids (camps, support groups)
- Consider a therapist who specializes in chronic illness
- Emphasize what they CAN do, not what they can’t
Part 4: For Partners and Spouses
The “One Kitchen, Two Diets” Challenge
Living with a partner who has celiac requires adjustment:
Options:
- Go fully gluten-free at home — Easiest, safest, most supportive
- Eat gluten only outside the home — Your partner can relax at home
- Strict separation system — More complex, higher risk of mistakes
Many couples choose option 1 or 2—it’s simply easier, and modern gluten-free food is good enough that you won’t feel deprived.
Supporting Without Smothering
DO:
- Learn to read labels (share the mental load)
- Call restaurants ahead to check on gluten-free options
- Defend them when others don’t take it seriously
- Keep safe snacks in your car/bag for emergencies
- Try new gluten-free restaurants together
DON’T:
- Hover or police their eating
- Express frustration about dietary restrictions in front of them
- Make them feel like a burden
- “Test” whether they really need to be this careful
- Eat their favorite gluten foods in front of them (at least at first)
Intimacy and Gluten
This might seem strange, but it matters:
- Kissing after eating gluten — Some people react, others don’t. Ask your partner.
- Lipstick/chapstick — Use gluten-free products if kissing is regular
- Toothpaste — Brush your teeth if you’ve eaten gluten (as a courtesy)
Social Situations as a Couple
You’re now their advocate in social situations:
At restaurants: Help vet the menu, speak up if something seems wrong At family dinners: Back them up when relatives don’t understand At work events: Bring safe food for both of you if needed
Part 5: Explaining Celiac to Family and Friends
The Short Version
“[Name] has celiac disease—an autoimmune condition where gluten damages their intestines. They have to avoid wheat, barley, and rye completely. Even a tiny amount makes them sick and causes internal damage. There’s no ‘just a little’ or ‘cheat days.’ It’s serious, but completely manageable with your support.”
When Family Doesn’t Take It Seriously
Unfortunately, this is common. You might hear:
- “A little won’t hurt.”
- “We’ve always eaten this way and were fine.”
- “That’s just a trendy diet.”
- “Can’t they just take a pill?”
Your response:
“This is a diagnosed autoimmune disease confirmed by medical testing. It’s not optional. If you can’t ensure the food is safe, we understand, but [Name] won’t be able to eat it. We can bring our own food—just please don’t be offended.”
If it continues:
- Bring all your own food to family events
- Eat before you arrive
- Consider whether this person should be around your child’s food unsupervised
Handling Holiday Meals
Option 1: Host at your house (safest)
- Control the entire kitchen
- Make favorite traditional dishes gluten-free (most can be adapted)
- Others can bring gluten items if kept completely separate
Option 2: Bring your own meal
- Prepare everything in your safe kitchen
- Heat in oven with foil covering (avoid microwaves others use)
- Bring enough to share so your loved one isn’t eating alone
Option 3: Work with the host
- Provide recipes and ingredient lists
- Ask them to prepare gluten-free dishes first, before any gluten cooking
- Verify ingredients of everything being served
- Have backup food just in case
Part 6: Cheat Cards for Caregivers
Safe/Unsafe Quick Reference
 Post this on your fridge - a quick visual guide for the whole family
Post this on your fridge - a quick visual guide for the whole family
| SAFE | UNSAFE |
|---|---|
| Rice, corn, potatoes | Wheat, barley, rye |
| Fresh meat/fish | Breaded or marinated meats |
| Fresh fruits & vegetables | Soups/sauces (check ingredients) |
| Most dairy (plain) | Beer, malt beverages |
| Eggs | Soy sauce (use tamari) |
| Certified gluten-free oats | Regular oats |
| Beans, nuts, seeds | Most bread, pasta, crackers |
Cross-Contact Checklist
- Separate toaster or toaster bags
- Dedicated cutting board (color-coded)
- Separate butter/condiments or squeeze bottles
- Gluten-free items stored above gluten items
- Separate colander
- Dedicated wooden utensils
- Clean surfaces before gluten-free prep
- Hand washing before handling gluten-free food
Restaurant Safety Questions
Ask before ordering:
- “Do you have a dedicated gluten-free prep area?”
- “Can the chef use clean utensils and cookware?”
- “Is the fryer oil shared with breaded items?”
- “Can you verify the ingredients in this dish?”
- “What gluten-free options do you recommend?”
Emergency Kit Contents
Keep in the car, bag, or locker:
- Gluten-free protein bars
- Nuts or seeds
- Fruit (fresh or dried)
- Rice cakes or gluten-free crackers
- Squeeze pouches (for kids)
- Safe candy (check labels)
Part 7: The Long Game—What to Expect
The First Year
Month 1-3: Steep learning curve
- Expect mistakes and accidental exposures
- Grocery shopping takes twice as long
- Lots of label reading and research
- Possible “withdrawal” symptoms or feeling worse before better
Month 4-6: Finding your rhythm
- You know which brands are safe
- Go-to restaurants identified
- Cooking becomes more confident
- Symptoms should be improving
Month 7-12: The new normal
- Gluten-free living feels routine
- Social situations become easier
- Health improvements are noticeable
- You’ve built a support network
Follow-Up Medical Care
Your loved one should have:
- Initial follow-up: 3-6 months post-diagnosis (check antibody levels)
- Annual appointments: Monitor healing, check nutrients
- DEXA scan: Baseline and periodic bone density tests
- Nutritional testing: Iron, B12, vitamin D, calcium, folate
Watching for Other Autoimmune Conditions
Celiac disease increases risk of other autoimmune conditions:
- Type 1 diabetes
- Thyroid disorders (Hashimoto’s, Graves’)
- Rheumatoid arthritis
- Sjögren’s syndrome
Regular check-ups and awareness of symptoms help catch these early.
Should Other Family Members Be Tested?
Yes. First-degree relatives (parents, siblings, children) have a 10-15% chance of having celiac disease.
Even without symptoms, testing is recommended because:
- Silent celiac causes damage without symptoms
- Early detection prevents complications
- Some symptoms are so normalized they’re not recognized
Part 8: Taking Care of Yourself Too
Caregiver Burnout Is Real
If you’re the main meal preparer and safety monitor, you’re carrying a significant mental load. Signs of burnout:
- Resentment about the extra work
- Exhaustion from constant vigilance
- Anxiety about making mistakes
- Frustration when others don’t help
Ways to Protect Your Own Well-being
- Share the responsibility — Teach other family members to cook safely
- Batch cook — Prepare safe meals in advance
- Find easy wins — Stock up on safe convenience foods for tired days
- Connect with other caregivers — Parent groups, online forums
- Take breaks — Let someone else handle meals sometimes
Building Your Support Team
- Dietitian: Find one experienced in celiac disease
- Gastroenterologist: For ongoing medical management
- Mental health support: For you and your loved one if needed
- Online communities: Facebook groups, Reddit, local celiac groups
- School staff, family members: Train them to help
Part 9: The Bright Side
They Can Live a Completely Normal Life
With proper management, someone with celiac can:
- Eat delicious food
- Travel anywhere in the world
- Play sports, go to college, have careers
- Have children (and breastfeed safely)
- Enjoy social occasions
- Live a long, healthy life
Modern Gluten-Free Options Are Excellent
We’re living in the best era for gluten-free eating:
- Restaurant awareness is at an all-time high
- Gluten-free products are available everywhere
- Quality has improved dramatically
- More naturally gluten-free cuisines are popular (Thai, Mexican, Indian)
You’re Giving Them a Gift
By learning about celiac disease and taking it seriously, you’re:
- Protecting their health
- Validating their experience
- Showing them they’re worth the effort
- Teaching them they deserve to be safe
- Modeling advocacy they can use for themselves
Connection and Understanding
Many families report that navigating celiac disease together brought them closer. The shared experience of:
- Learning together
- Cooking together
- Problem-solving together
- Celebrating victories together
…creates bonds that wouldn’t exist otherwise.
Part 10: You’re Already Doing Great
The fact that you’re reading this guide means you care deeply about your loved one’s health and happiness. That’s the foundation everything else builds on.
Remember:
- You’ll make mistakes, and that’s okay
- Your loved one’s health will improve
- It gets easier with time
- You’re not alone in this
Welcome to the celiac caregiver community. We’re here for you too.
Sources
- Rubio-Tapia A, et al. “The prevalence of celiac disease in the United States.” American Journal of Gastroenterology. 2012.
- Sollid LM, et al. “Evidence for a primary association of celiac disease to a particular HLA-DQ alpha/beta heterodimer.” Journal of Experimental Medicine. 1989.
- Green PHR, Cellier C. “Celiac Disease.” New England Journal of Medicine. 2007.
- Celiac Disease Foundation. “What is Celiac Disease?” Accessed January 2026.
- Beyond Celiac. “School and Celiac Disease.” Accessed January 2026.
- Gluten Intolerance Group. “Gluten-Free Food Service Guidelines.” Accessed January 2026.