 Your first priority: learning to keep your food safe from cross-contact
Your first priority: learning to keep your food safe from cross-contact
First: Take a Breath
You just received a diagnosis that’s going to change how you eat for the rest of your life. That’s big. It’s okay to feel overwhelmed, scared, angry, relieved (finally an answer!), or all of the above.
Here’s what you need to know right now:
- Celiac disease is manageable
- You will feel better
- You’re not alone—3 million Americans have this condition
- The learning curve is steep at first, then it becomes second nature
This guide will walk you through everything—from understanding what’s happening in your body to explaining it to your confused relatives to the practical tricks that make daily life easier.
Part 1: Understanding What Celiac Disease Actually Is
The Simple Explanation
Celiac disease is an autoimmune condition where eating gluten causes your immune system to attack your small intestine.
When you eat gluten (a protein in wheat, barley, and rye), your body sees it as a threat and launches an immune response. But instead of attacking the gluten, your immune system attacks the lining of your small intestine—specifically the tiny finger-like projections called villi that absorb nutrients from food.
The result: damaged intestines, malabsorption of nutrients, and a whole cascade of symptoms that can affect virtually every system in your body.
Why This Matters
Your small intestine is where your body absorbs:
- Vitamins and minerals
- Proteins
- Fats
- Carbohydrates
- Basically everything your body needs to function
When the villi are damaged, you can eat a perfectly healthy diet and still be malnourished. This explains symptoms you might have experienced:
- Fatigue (iron, B12 deficiency)
- Brain fog (nutrient deficiencies)
- Bone pain (calcium, vitamin D deficiency)
- Digestive issues (damaged intestinal lining)
- Skin problems, joint pain, mood changes, and dozens of other symptoms
The Good News
Your intestines can heal. Once you remove gluten from your diet, the immune attack stops, and your villi can regenerate. Most people see significant improvement within weeks to months, with full healing typically occurring within 1-2 years.
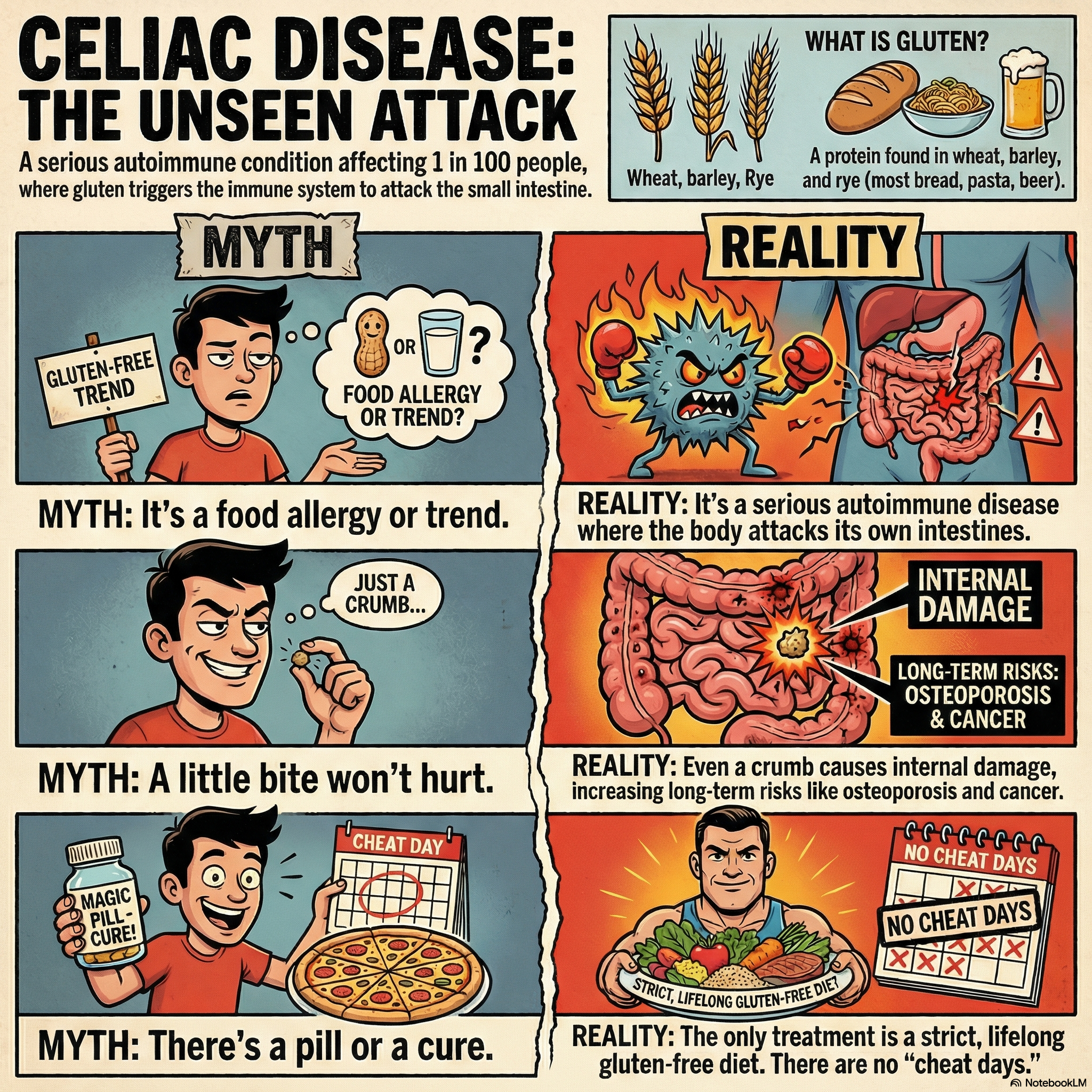 Celiac disease is an autoimmune condition - your immune system attacks your own intestines when gluten is present
Celiac disease is an autoimmune condition - your immune system attacks your own intestines when gluten is present
Part 2: Explaining Celiac to Others
The “Elevator Pitch” (30 Seconds)
Use this when someone asks “What’s celiac disease?”
“I have an autoimmune disease where my immune system attacks my intestines when I eat gluten—that’s a protein in wheat, barley, and rye. It’s genetic and there’s no cure, so I have to avoid gluten completely for the rest of my life. Even a tiny amount—like a breadcrumb—causes damage and makes me sick.”
The “This Is Serious” Explanation
Use this when someone isn’t taking it seriously:
“Celiac disease isn’t a food preference or a diet trend. It’s a serious autoimmune condition, like Type 1 diabetes or rheumatoid arthritis. When I eat gluten, my immune system attacks my intestines and causes real, measurable damage. Continued exposure increases my risk of osteoporosis, other autoimmune diseases, and certain cancers. The only treatment is a strict gluten-free diet—there’s no pill I can take, no ‘cheat days,’ and no amount that’s safe.”
The “Why I Can’t Just Pick Off the Croutons” Explanation
Use this when someone doesn’t understand cross-contact:
“Once gluten touches my food, I can’t eat it—even if I remove the visible gluten. Here’s why: gluten is a sticky protein that leaves invisible residue on everything it touches. Studies show that even 10-20 milligrams of gluten (about 1/100th of a slice of bread) can cause intestinal damage in people with celiac disease. That’s why I can’t just pick off the croutons or scrape off the sauce. The damage is already done.”
Addressing Common Misconceptions
“But you don’t look sick!”
“Celiac disease is often called an ‘invisible illness.’ The damage happens inside my intestines where you can’t see it. Many people with celiac have been sick for years without knowing why—the average diagnosis takes 6-10 years.”
“Can’t you have just a little?”
“No. For someone with celiac, there’s no safe amount of gluten. Even tiny amounts that wouldn’t make me visibly sick still cause intestinal damage. It’s like asking someone with a peanut allergy to have ‘just a little’ peanut.”
“Is this like being gluten-free by choice?”
“No—and this is an important distinction. Some people choose to avoid gluten for various reasons, and they might be fine with a little cross-contact. For me, it’s a medical necessity. I don’t have a choice, and my requirements are much stricter. I need food prepared with separate equipment, not just ‘gluten-free ingredients.’”
“My friend has celiac and they eat bread sometimes.”
“They might have a different condition (like gluten sensitivity), or they might not realize the damage they’re causing. Some people with celiac don’t have obvious symptoms but are still experiencing intestinal damage. It’s called ‘silent celiac’—no symptoms doesn’t mean no harm.”
Part 3: The Must-Know Essentials
What Contains Gluten
Always contains gluten:
- Wheat (including spelt, kamut, farro, durum, semolina, einkorn)
- Barley (including malt, malt vinegar, malt flavoring)
- Rye
- Triticale (wheat-rye hybrid)
- Most conventional oats (due to cross-contact)
Hidden gluten sources:
- Soy sauce (contains wheat—use tamari or coconut aminos)
- Many salad dressings and sauces
- Beer and malt beverages
- Some medications and supplements
- Communion wafers
- Play-Doh (don’t let kids put it in their mouths)
- Some lipsticks and lip balms
- Imitation crab and some processed meats
What’s Naturally Gluten-Free
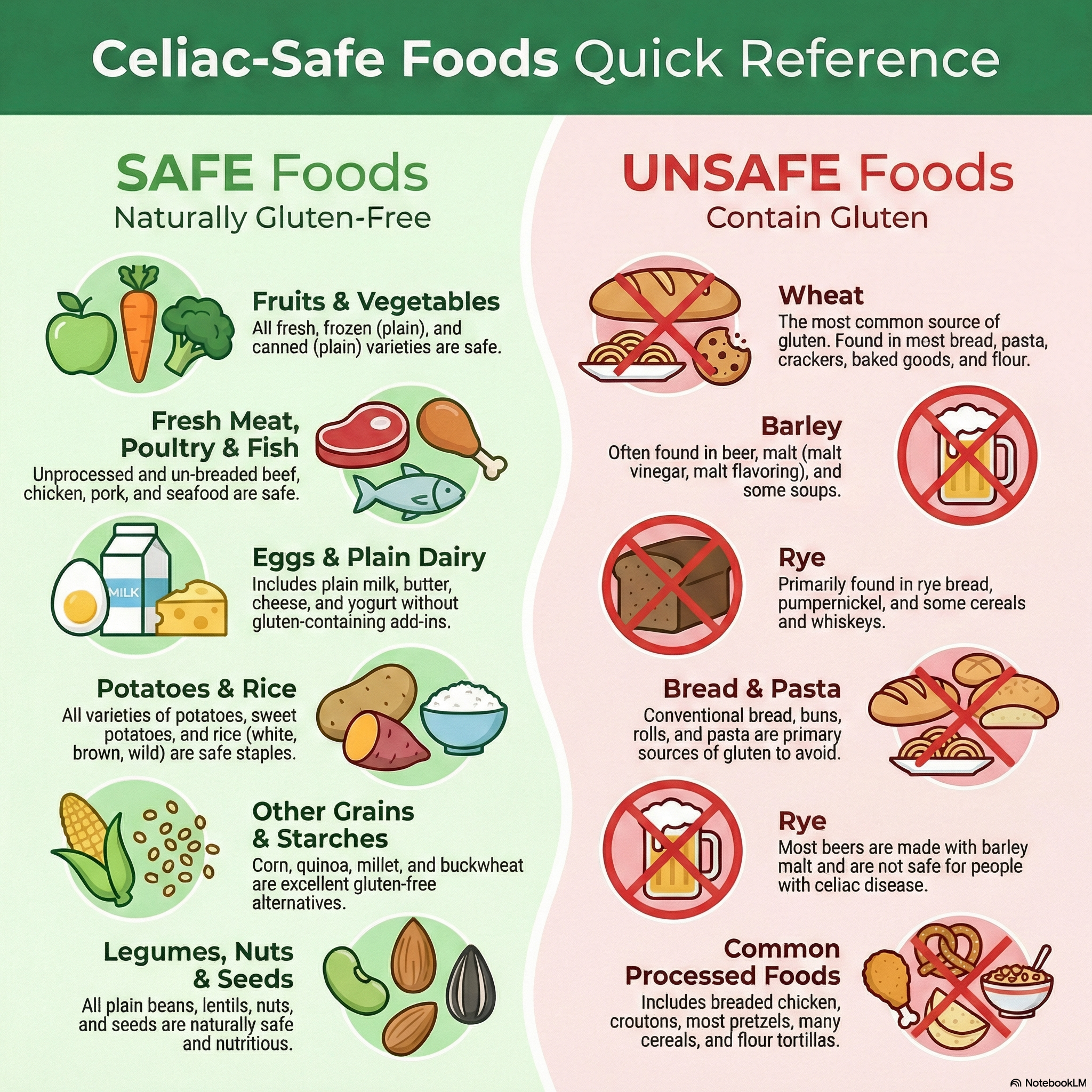 Your at-a-glance guide to safe and unsafe foods
Your at-a-glance guide to safe and unsafe foods
You CAN eat:
- All fruits and vegetables
- Plain meat, poultry, fish, and seafood
- Eggs
- Dairy (milk, cheese, butter, plain yogurt)
- Rice (all varieties)
- Corn and cornmeal
- Potatoes
- Beans and legumes
- Nuts and seeds
- Certified gluten-free oats
- Quinoa, buckwheat, millet, amaranth, teff, sorghum
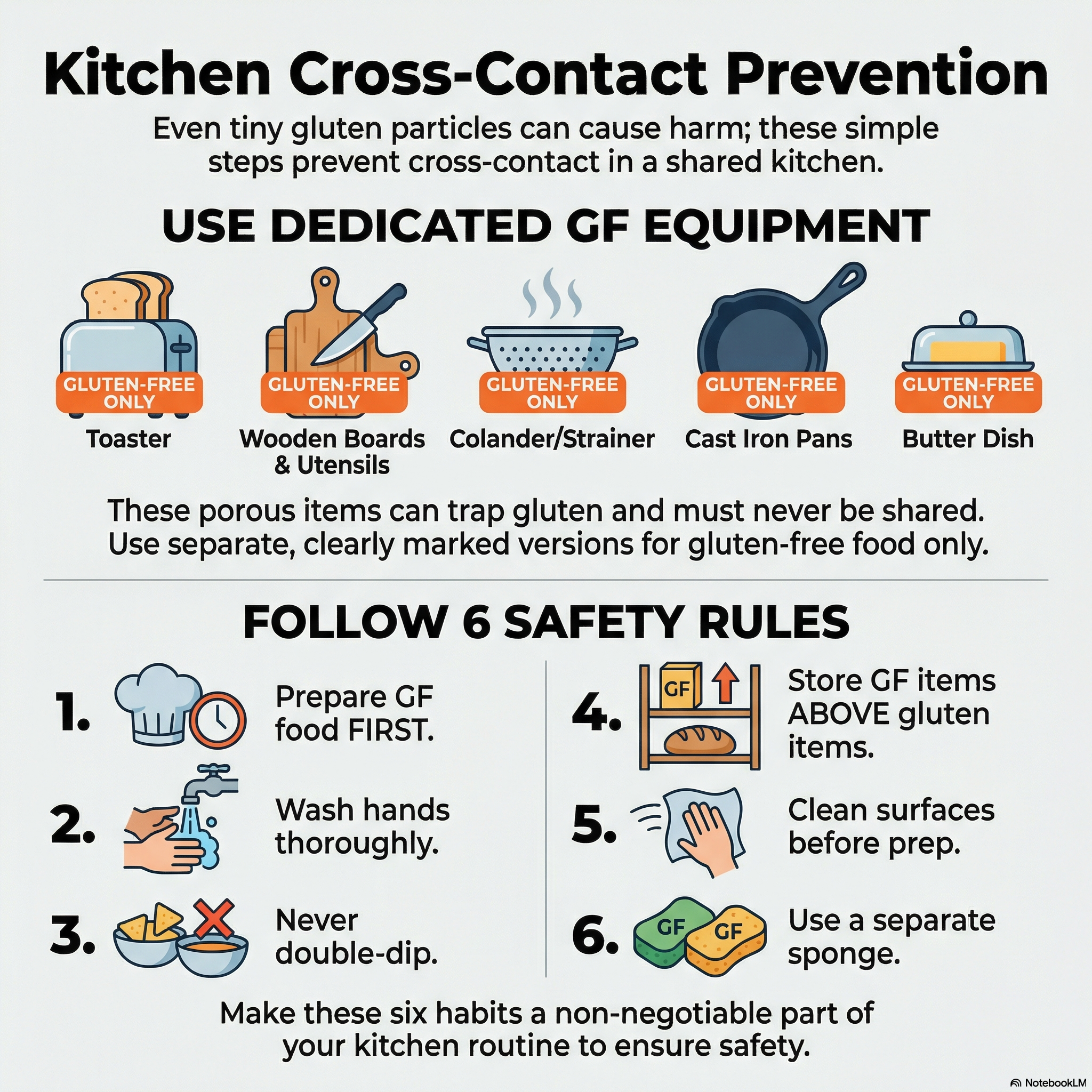
The Cross-Contact Problem
Cross-contact (sometimes called cross-contact) happens when gluten-free food touches gluten or surfaces/equipment that touched gluten.
Common cross-contact sources:
- Shared toasters
- Shared butter or peanut butter jars (crumbs)
- Shared cooking oil (especially fryers)
- Cutting boards and wooden utensils
- Colanders and strainers
- Shared grills
- Flour dust in the air (settles on surfaces)
The solution: Dedicated equipment for gluten-free cooking, or thorough cleaning between uses.
Label Reading 101
In the US:
- “Gluten-Free” on FDA-regulated foods means <20 ppm gluten
- Wheat must be declared as an allergen
- Barley and rye are NOT required to be declared
What to look for:
- “Certified Gluten-Free” (third-party tested, often <10 ppm)
- GFCO certification logo (tested <10 ppm)
- “Made in a dedicated gluten-free facility”
Red flags:
- “May contain wheat”
- “Made on shared equipment with wheat”
- “Made in a facility that processes wheat”
- Malt (unless specified as gluten-free)
- “Natural flavors” (usually fine, but can occasionally contain gluten)
Part 4: Cheat Cards
Quick Reference: Safe vs. Unsafe
 Keep this handy - your visual guide to safe and unsafe foods
Keep this handy - your visual guide to safe and unsafe foods
| SAFE | UNSAFE |
|---|---|
| Rice, corn, potatoes | Wheat, barley, rye |
| Certified gluten-free oats | Regular oats |
| Fresh meat/fish/poultry | Breaded or marinated meats |
| Fresh fruits/vegetables | Anything with sauce (check first) |
| Most dairy | Beer, malt beverages |
| Eggs | Soy sauce (use tamari) |
| Beans, nuts, seeds | Most baked goods |
| Wine, most spirits | Communion wafers |
| Tamari, coconut aminos | Regular soy sauce |
Restaurant Survival Card
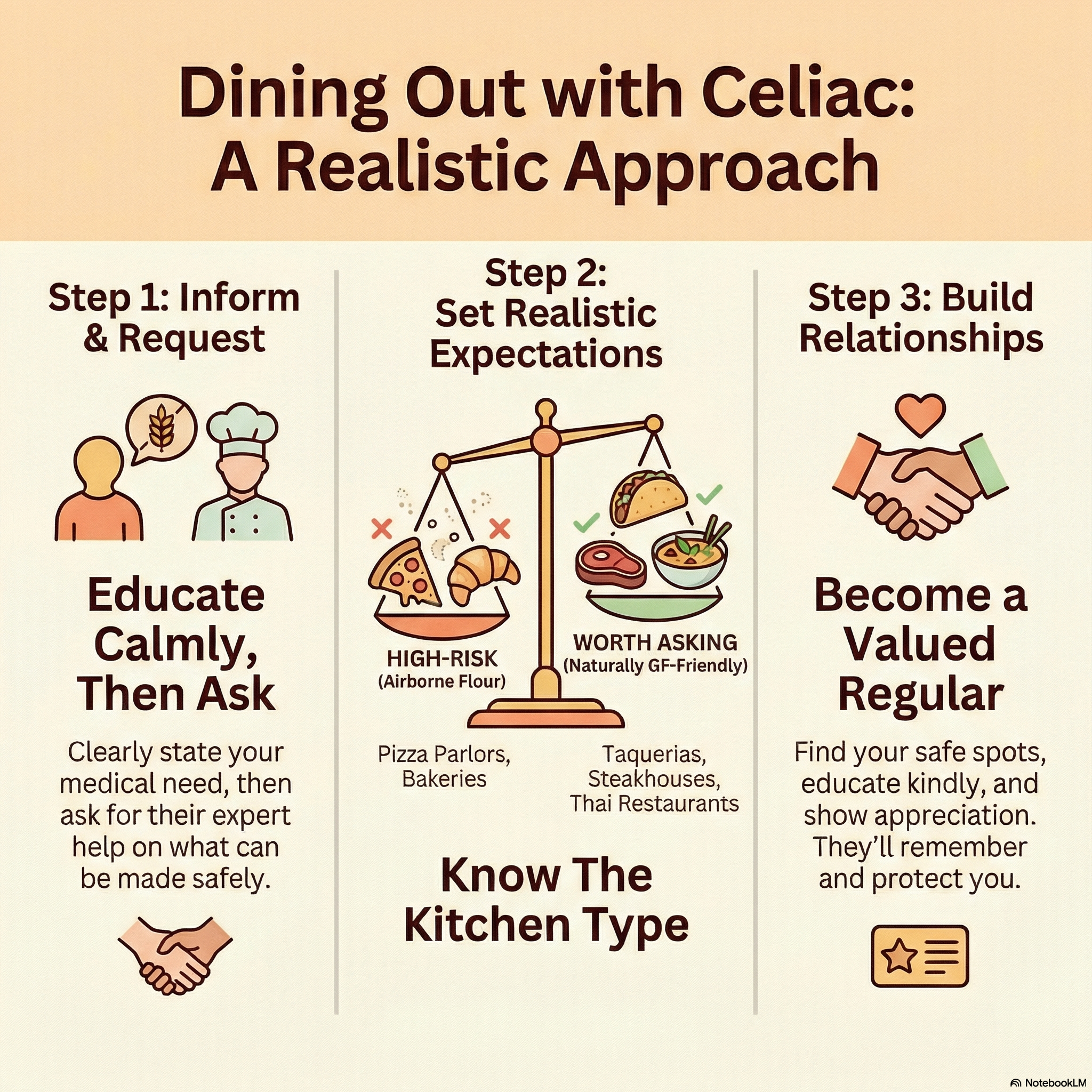 Educate, collaborate, build relationships - the key to dining out safely
Educate, collaborate, build relationships - the key to dining out safely
Say this when ordering:
“I have celiac disease—not a preference, a medical condition. I need food prepared without any gluten, using clean equipment. Can you accommodate that?”
Questions to ask:
- “Do you have a separate prep area for gluten-free orders?”
- “Will you use clean utensils and a clean cooking surface?”
- “Is there shared fryer oil with breaded items?”
- “Can the chef change gloves before preparing my food?”
Safer choices at restaurants:
- Grilled proteins without marinade (ask for oil and salt only)
- Baked potatoes (no cross-contact from butter)
- Steamed vegetables
- Salads with oil and vinegar (no croutons, dressing on side)
- Rice dishes (verify no soy sauce or shared cooking surface)
Kitchen Setup Essentials
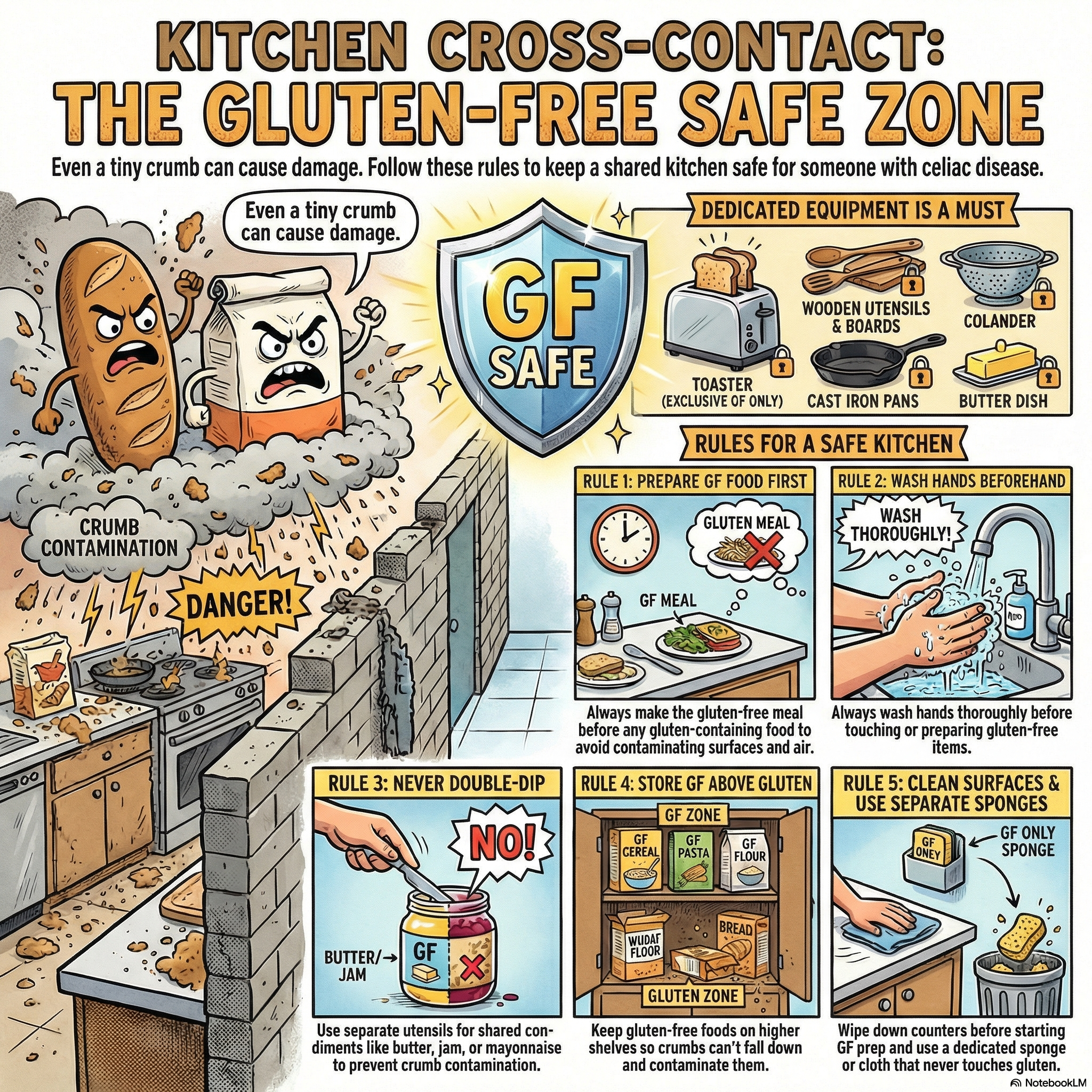 Your kitchen needs dedicated gluten-free zones to stay safe
Your kitchen needs dedicated gluten-free zones to stay safe
Must-have dedicated items:
- Toaster (or toaster bags)
- Cutting board
- Colander/strainer
- Wooden spoons and utensils (they harbor gluten)
- Butter dish or squeeze bottle
- Condiment containers (or use squeeze bottles)
Can be shared if thoroughly washed:
- Metal pots and pans
- Metal utensils
- Glass and ceramic dishes
- Stainless steel appliances
Emergency Snack Kit
Keep these on hand for when you’re caught without safe food:
- Nuts or seeds
- Cheese sticks or string cheese
- Fresh fruit (apples, bananas)
- Gluten-free protein bars (RXBARs, KIND bars—check labels)
- Rice cakes
- Single-serve nut butter packets
Part 5: Let’s Have the Real Talk
This Is Going to Be Hard Sometimes
I’m not going to sugarcoat it. Here’s what you’ll face:
Social challenges:
- Feeling awkward at restaurants when you need special accommodations
- Friends and family who don’t understand or take it seriously
- Missing out on shared food experiences (birthday cake, pizza parties)
- The emotional weight of always having to think about food
Practical challenges:
- Gluten-free products cost 2-3x more than regular equivalents
- Limited options at many restaurants, airports, and events
- The constant mental load of reading every label
- Travel requires significant planning
- Dating and social eating become more complicated
Emotional challenges:
- Grieving foods you can no longer eat
- Frustration when you get “glutened” despite being careful
- Anxiety about cross-contact
- Feeling like a burden when others have to accommodate you
The Symptoms You Might Experience
When you get accidentally exposed (“glutened”):
- Symptoms vary hugely between people
- Common reactions: digestive issues, fatigue, brain fog, headaches, joint pain, skin issues, mood changes
- Symptoms can last hours to weeks
- There’s no way to speed up recovery—just rest, hydrate, and wait it out
During the healing period:
- You might actually feel worse before you feel better (as your gut adjusts)
- Some people experience withdrawal-like symptoms
- Nutrient deficiencies may take months to correct
The Hidden Struggles No One Talks About
The hypervigilance is exhausting. Always reading labels, always asking questions, always being “that person” at restaurants. It takes a mental toll that people without food restrictions don’t understand.
You’ll make mistakes. Everyone does, especially in the first year. You’ll eat something you thought was safe and suffer for it. Don’t beat yourself up—it’s part of the learning curve.
Some people won’t believe you. You’ll encounter people who think you’re being dramatic, that you have an eating disorder, or that you’re following a fad. Their ignorance is not your problem.
Restaurants will mess up. Even restaurants with gluten-free menus. Even restaurants that claim to understand. You’ll have to decide how much risk you’re comfortable with.
Part 6: The Bright Side (Yes, There Is One)
Your Health Will Improve
This is the biggest bright side: you finally have an answer, and the solution is within your control.
Many people with celiac spend years—often decades—feeling terrible without knowing why. Doctors might have told you it was IBS, anxiety, or “just stress.” Now you know the cause, and you can do something about it.
What you might experience:
- More energy than you’ve had in years
- Clearer thinking (goodbye, brain fog)
- Better digestion
- Improved mood
- Healthier skin, hair, and nails
- Fewer headaches and joint pain
- Better nutrient absorption overall
You’ll Discover a Whole Community
You’re joining a community of millions of people who understand exactly what you’re going through. We’ve all been there—the learning curve, the mistakes, the frustrations, and the victories.
Resources:
- Celiac Disease Foundation
- Beyond Celiac
- Gluten Intolerance Group
- Local celiac support groups
- Online communities (Reddit r/Celiac, Facebook groups)
Gluten-Free Food Has Never Been Better
The gluten-free market has exploded. Twenty years ago, gluten-free bread was cardboard. Today, there are excellent options for almost everything:
- Bread that actually tastes like bread
- Pasta that doesn’t turn to mush
- Pizza crusts that rival the real thing
- Baked goods that could fool anyone
Brands to explore:
- Canyon Bakehouse (bread)
- Barilla, Jovial, or Banza (pasta)
- Siete or Caulipower (tortillas, pizza)
- King Arthur or Bob’s Red Mill (baking mixes)
- Simple Mills (crackers, cookies)
You’ll Become a Better Cook
Necessity is the mother of invention. Many people with celiac become excellent home cooks because:
- You learn to cook from scratch (safer and cheaper)
- You experiment with naturally gluten-free cuisines (Mexican, Thai, Indian, Japanese)
- You discover new ingredients you never would have tried
It Gets Easier
I promise you this: what feels impossible now will become automatic.
The first trip to the grocery store takes forever. The first restaurant meal is stressful. The first holiday dinner requires planning a week in advance.
But after a few months:
- You’ll know which brands are safe without checking
- You’ll have go-to restaurant orders that work
- You’ll have perfected your favorite gluten-free recipes
- Explaining your condition will become second nature
One day, you’ll realize you went the whole day without thinking about celiac. That’s the goal.
Part 7: Your First Week Action Plan
Day 1-2: Clean Out the Kitchen
- Remove obvious gluten (bread, pasta, crackers, cereal)
- Don’t worry about hidden sources yet—start with the basics
- Get dedicated butter, peanut butter, and condiments
- Buy or designate a separate toaster
Day 3-4: Stock Up on Basics
- Gluten-free pasta
- Certified gluten-free oats (if you eat oats)
- Rice and potatoes
- Fresh produce, meat, eggs, dairy
- A few gluten-free convenience items for when you’re tired
Day 5-6: Learn to Read Labels
- Practice at the grocery store
- Download the Find Me Gluten Free app
- Save a list of safe brands on your phone
Day 7: Make One Great Meal
- Cook something delicious that happens to be gluten-free
- Not “gluten-free pasta with gluten-free sauce”—something naturally gluten-free that celebrates whole ingredients
- Grilled steak with roasted vegetables, fish tacos on corn tortillas, Thai curry with rice, a beautiful salad
Part 8: What About Medications and Supplements?
Prescription Medications
- Gluten can be used as a filler in some medications
- Always tell your pharmacist you have celiac disease
- Ask them to check the inactive ingredients
- Request alternatives if needed
- Resources: GlutenFreeDrugs.com
Supplements
- You may need supplements during healing (iron, B12, vitamin D, calcium)
- Work with your doctor to check your nutrient levels
- Look for certified gluten-free supplements
- Some supplements to consider: Designs for Health, Pure Encapsulations, Thorne (all certified GF)
Part 9: Managing Your Mental Health
It’s Normal to Grieve
You’re allowed to mourn the foods you can’t eat anymore. The convenience of grabbing whatever you want. The spontaneity of eating out anywhere. Give yourself permission to feel sad about it.
Dealing with Anxiety
Food anxiety is common with celiac. If you find yourself:
- Afraid to eat anything
- Obsessively checking labels
- Avoiding all restaurants and social eating
- Losing significant weight due to fear of eating
…please talk to a mental health professional who understands chronic illness. There’s a line between appropriate vigilance and food-related anxiety disorders.
Building Resilience
- Focus on what you CAN eat, not what you can’t
- Find celiac-safe restaurants and make them your go-tos
- Connect with others who understand
- Celebrate wins (great meals, successful events, improved health)
Part 10: You’ve Got This
Celiac disease is a significant diagnosis. It changes how you eat, how you socialize, and how you think about food. But it’s also:
- Completely manageable
- The key to better health
- A path to discovering delicious new foods
- An entry into a supportive community
You’re not starting over. You’re just starting a new chapter—one where you finally know what was making you sick and have the power to fix it.
Welcome to the celiac community. We’re glad you’re here.
Sources
- Rubio-Tapia A, et al. “The prevalence of celiac disease in the United States.” American Journal of Gastroenterology. 2012.
- Catassi C, et al. “A prospective, double-blind, placebo-controlled trial to establish a safe gluten threshold for patients with celiac disease.” American Journal of Clinical Nutrition. 2007.
- Green PHR, Cellier C. “Celiac Disease.” New England Journal of Medicine. 2007.
- Celiac Disease Foundation. “What is Celiac Disease?” Accessed January 2026.
- Beyond Celiac. “The Gluten-Free Diet.” Accessed January 2026.
- FDA. “Gluten-Free Labeling of Foods.” Accessed January 2026.